#Pulsemdx is an educational blog which runs alongside Twitter.
A new ECG “quizz” is launched every Monday evening.
Any discussions generated with be archived for summary and reflection, on the following interim @Pulsemdx
A 56yrs man who rarely attends, but he woke in the small hours of the night with ‘indigestion’. The pain hasn’t got any worse, but it’s niggled on for several hours now, so his wife booked the appointment and insisted he came down to have an ECG before work.
He’s never really suffered with indigestion before, but has no cardiac history or risk factors.
He looks a little unsettled and restless, but nothing else of note. Apart from a slight tachycardia, his pulse is normal, and BP borderline elevated (he’s visibly a bit anxious).
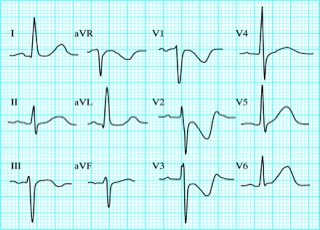
The ECG shows:
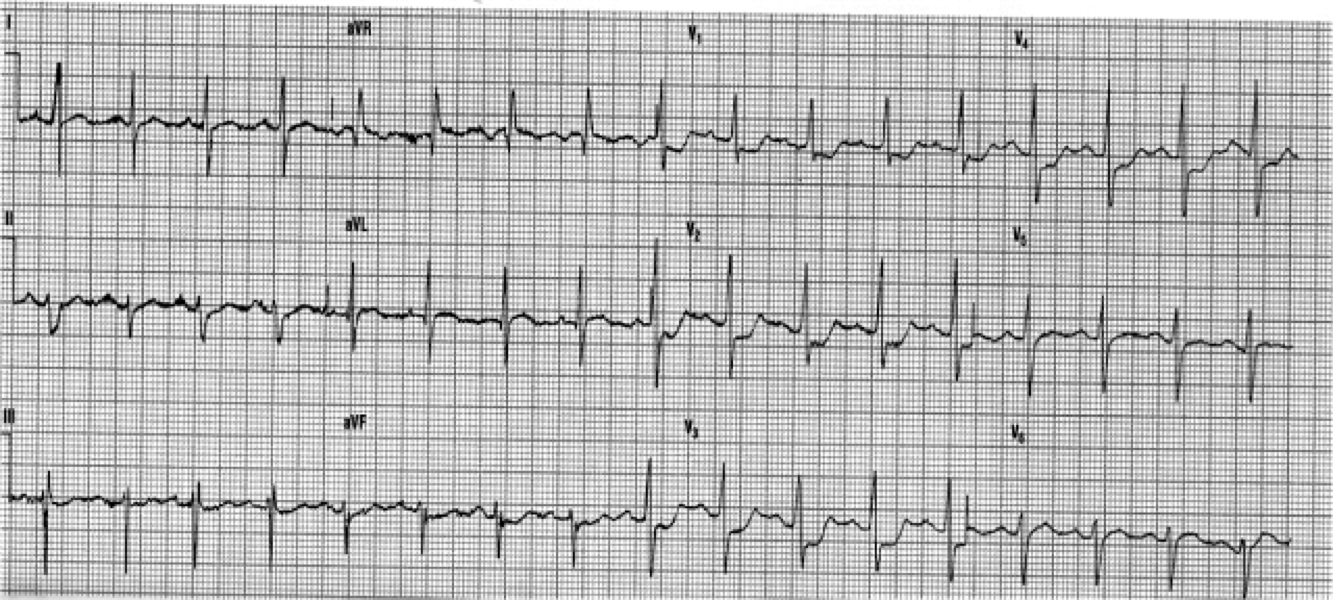
What does the ECG show? (Stick to describing the ST changes only).
The ECG shows 2-3mm of horizontal/downsloping ST depression in leads V1-4
At first glance I would have felt this showed anterior ischaemia.
But, bear in mind, he has ongoing pain, at rest. This has to be assumed to be Acute Coronary Syndrome until proven otherwise.
In accordance with NICE Guidelines for new onset chest pain, and in order appropriate to the circumstances, offer:
- Pain relief
- Aspirin
- Other Therapeutic interventions
- Pulse oximetry (supplement O2 only if % SAO2 indicates)
- Monitor until ambulance arrives (GP) or diagnosis confirmed (Hospital)
On arrival at A&E, serial troponins were taken, and the posterior ECG leads (V7-9) were monitored.
A subsequent diagnosis of Posterior MI was made.
Posterior Myocardial Infarction
With Acute MI, the presence of persistent ischaemic pain, indicates that still viable areas of ischaemic and injured myocardium are in danger of necrosis.
It is outwith the concept of this forum, to go into management of Acute Coronary Syndrome (ACS) in any detail, but everyone should make themselves familiar with the NICE Guideline “Chest Pain of Recent Onset” (CG95).
Pages 1-9 of the Quick reference guide linked above, deals with ACS, whereas pages 10 onwards, deal with stable angina.
In STEMI, the ECG leads which are orientated to the area supplied by the affected coronary artery will reveal the ST elevation. And so, the area of infarction can be determined by which leads of the ECG are affected:
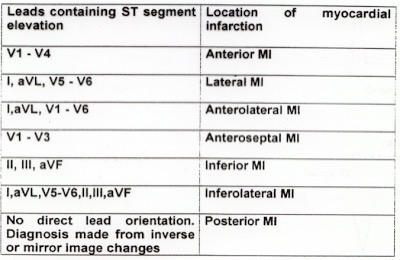
And it follows, that the coronary artery affected in Acute Myocardial Infarction, is determined by the location of the MI :
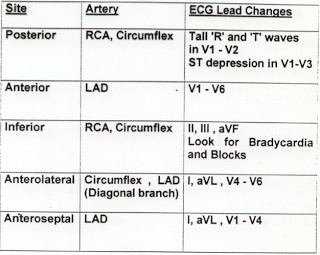
Of course, reliance on ST elevation to diagnose STEMI, assumes we are viewing the affected myocardium from the front. What if the ST elevation is in the posterior myocardial wall?
If ST depression is present in leads V1-V3, with ongoing chest pain, then recording of the posterior leads (V7,V8,V9) will be invaluable.
The posterior leads are placed on the posterior chest wall:
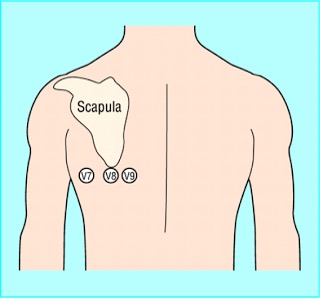
Of course,the recordings from the 3 posterior leads will therefore be a mirror-image of V1-3 :

And so, the posterior ST elevation becomes obvious.
Posterior MI is often a bit of an enigma to GP’s and students, and I’m sure we all recall been told to flip the ECG paper upside down, and view form the back. When lacking precious time/ability to monitor the posterior leads, this method can still be invaluable – it’s just remembering to think of it!
Hope that helps a little.
Looking forward to any more gems of education on posterior MI’s (for me) from anyone who’d like to add a comment! 🙂
Thank you.